Interim results of the ACROBAT study suggest that increasing microchimerism and loss of complete chimerism may indicate relapse risk in patients with acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS). The findings were presented in an oral abstract1 at the 2025 Transportation and Cellular Therapy Tandem Meetings of ASTCT and CIBMTR in Honolulu, Hawaii.
The ACROBAT study is a prospective, multicenter, observational cohort study that enrolled patients 18 years and older who were eligible for allogeneic hematopoietic stem cell transplantation (HSCT) with AML, acute lymphoblastic leukemia (ALL), and MDS.2
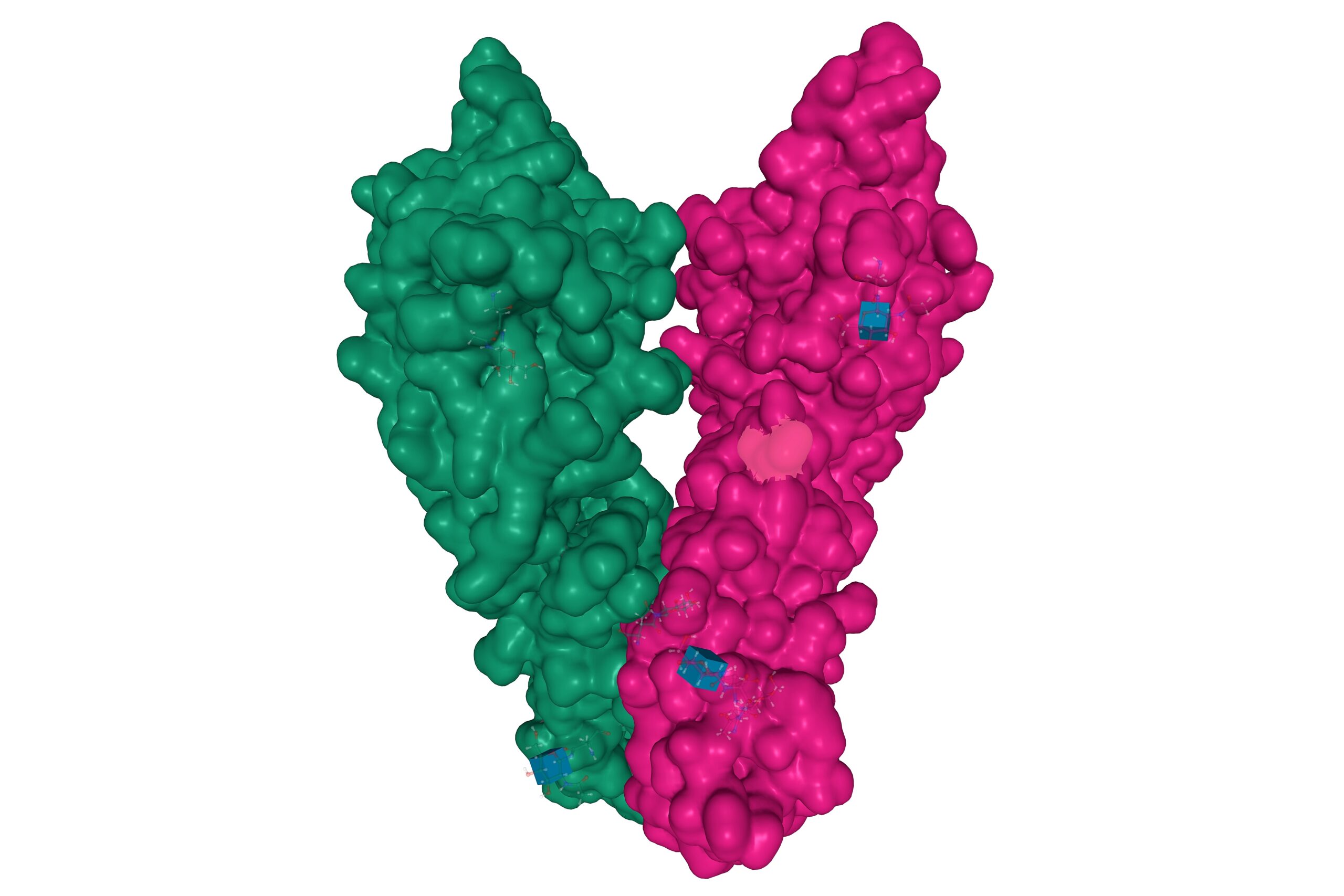
To measure microchimerism for relapse prediction, the investigators analyzed blood or bone marrow samples using the AlloHeme® microchimerism test, a next-generation sequencing technology, which measures single nucleotide polymorphisms to assess donor and recipient cell proportions after HCT.
The AlloHeme® microchimerism test has a limit of detection of 0.04% for unrelated donors and 0.07% for related donors, according to the study investigators. Increasing microchimerism was defined as ≥0.2% increase in recipient chimerism between two consecutive time points. Complete chimerism was defined as donor chimerism ≥99.8% at three months after transplantation, and relapses were defined using CIBMTR criteria.
ACROBAT interim analysis
In this interim analysis, the researchers report on CD33 increasing microchimerism in 235 patients with AML and MDS at a median follow-up of 14 months. The researchers reported 7% relapse and 23% nonrelapse mortality in this patient subgroup.
Analyses at three and six months showed that patients with increasing microchimerism had a significantly higher risk of relapse compared with those without increasing microchimerism (P= 0.016 and P= 0.001). A time-varying effects model found that patients with increasing microchimerism had a 35.2 times higher risk of relapse (CI, 15.5-80.3; P<0.001).
An increasing microchimerism threshold of ≥0.2% had 93% sensitivity, 76% specificity, a 98% negative predictive value and a 47% positive predictive value for relapse prediction.
The median time from increasing microchimerism detection to relapse was 50 days in 63% of relapsing patients (n=25).
Patients who never achieved CD33 complete chimerism (n=30) had a 12.2 times higher relapse risk than those who achieved complete chimerism (n=199). Those who achieved complete chimerism but later lost it (n=60) had a 27.5 times higher relapse risk than those who maintained CC (n=139). The median time from loss of complete chimerism to relapse was 153 days (n=27, 68% of relapses).
“Microchimerism using AlloHeme is an accurate and sensitive test for monitoring relapse in post-allo HCT AML and MDS patients with a clinically meaningful lead time to relapse prediction,” the investigators, led by Monzr Al Malki, MD, of the Department of Hematology and HCT at the City of Hope National Medical Center in Duarte, California, wrote in the oral abstract.
Reference
- Al Malki MM, Sobecks R, Cutler Cory. Transportation and Cellular Therapy Tandem Meetings of ASTCT and CIBMTR. CD33 Microchimerism Assessment By Alloheme Predicts Early Relapse in Patients with AML/MDS—Interim Results from the Acrobat Multicenter Study. Abstract #7. Tandem Meetings | 2025 Transportation and Cellular Therapy Tandem Meetings of ASTCT and CIBMTR; February 12-15; Honolulu, Hawaii
- ClinicalTrials.gov. Study of microchimerism and relapse in post-transplant patients (ACROBAT). Identifier NCT04635384. Updated January 23, 2024. Accessed February 12, 2025.