My diagnosis with Paroxysmal Nocturnal Hemoglobinuria Paroxysmal Nocturnal Hemoglobinuria: (par-uk-SIZ-muhl nok-TURN-uhl hee-muh-gloe-buh-NYOOR-ee-uh) A rare and serious blood disease that causes red blood cells to break apart. Paroxysmal means sudden and irregular. Nocturnal means at night. Hemoglobinuria means hemoglobin in the urine. Hemoglobin is the red part of red blood cells. A… (PNH) was a lot to handle, as is any diagnosis of any kind. I could talk forever in circles about the experience of my diagnosis and how it changed everything for me. For the beginning of my story, I will specifically focus on my medical diagnosis of PNH.
Here are the symptoms I was showing before my diagnosis: I was exhausted, all the time. I could not do any athletic activity without being incredibly shaky for hours after, sometimes having to lay around the entire next day. I can remember lying on my couch after surfing and thinking if I stood up my legs wouldn’t be able to hold me up. Dark urine, I mean dark as in black. This happened to me twice before I was diagnosed. I would get insane abdominal pain at times, similar to cramping in the abdomen. I had a very yellow tint to my eyes and pale skin.
I’ll start at the beginning. In early 2008, at 19 years old, I began to experience overwhelming exhaustion, so I visited my physician. I was diagnosed with mononucleosis. I took it easy as the doctor recommended, but I never felt normal again. In the summer of 2008, I was admitted to the hospital with dehydration and heat exhaustion.
Upon drawing lab work the doctors found I was slightly anemic, with a hemoglobin hemoglobin: A protein in the red blood cells. Hemoglobin picks up oxygen in the lungs and brings it to cells in all parts of the body. somewhere around 11gm/ dL. Hemoglobin is the part of red blood cells that carries the oxygen throughout the body (Cleveland Clinic, 2018). Cleveland Clinic (2018) defines normal range for hemoglobin in males as 14.0-17.5 gm/dL, for females 12.3-15.3 gm/dL. During the hospital stay, either night one or two, I woke up at night to urinate and my urine was black (this is the first time that had ever happened to me). It was terrifying.
The physicians told me due to my dehydration my body had broken down muscle and blood cells; they monitored my kidney function, collected 24-hour urine, and gave IV hydration. After the stay, I was even sent to an oncologist oncologist: (on-KAH-luh-jist) A doctor who specializes in the treatment and prevention of cancer. /hematologist to follow up on my anemia anemia: (uh-NEE-mee-uh) A condition in which there is a shortage of red blood cells in the bloodstream. This causes a low red blood cell count. Symptoms of anemia are fatigue and tiredness. . I remember the consultation with the oncologist, I remember being told I was anemic, but I did not have anything to worry about, no cancers, no blood diseases.
In discussing this with my mom while writing this, she stated that the hematologist hematologist: (hee-muh-TOL-uh-jist) A doctor who specializes in treating blood diseases and disorders of blood producing organs. I had seen monitored my blood counts for a few months and that he had determined my levels lived in this lower range (I did not remember this, however being curious have reached out to his office for records to see exactly what my diagnosis was— will update when I know more). Let’s stop— anemia, black urine, exhaustion. Did I have PNH in 2008? I would bet so.
After my symptoms continued over the next few years, I saw multiple doctors. All the tests came back negative, except for my primary care physician diagnosing me with hypoglycemia and anxiety. Oncology- slightly anemic, Cardiology- normal EKG, normal stress test. By 2010 I stopped seeing doctors, I pushed through. When I felt like I couldn’t stand, I told myself it was just anxiety. When I felt like I couldn’t exercise, I told myself I was weak and kept going. If someone else could do something, I could do it too. I spent many days keeping up with friends, and many of the next days recovering in bed.
Fast forward to April 2014, my wife and I were getting ready to start travel nursing, and for our new jobs we had to get physicals. Our physician ran lab work that showed my hemoglobin was critically low at 7.7 gm/dl. Remember that Hemoglobin is the part of red blood cells that carries the oxygen throughout the body (Cleveland Clinic, 2018). And also remember that the Cleveland Clinic (2018) defines normal range for hemoglobin in males as 14.0-17.5 gm/dL, for females 12.3-15.3 gm/dL.
Welp! Now there was a clear reason why I felt so horrible all the time. My body was working with much lower blood counts than it should have been. I was scheduled to see a GI doctor and a hematologist. Initially, my physician thought maybe this was GI related. I had a stressful job, drank coffee, and did not sleep as much as I should so the thought was maybe I had a slow bleeding ulcer? I also remember them thinking possibly celiac disease?
My hematologist diagnosed me with iron deficiency anemia and started me on folic acid folic acid: See folate. and iron. I started taking the folic acid and iron right away. He was sure that soon we would see a boost in iron levels, which would help to create more blood cells, and then blood counts would normalize. I had an EGD/ colonoscopy done which showed that I had no signs of bleeding and no celiac disease, so iron deficiency anemia was the diagnosis.
After a few weeks on the iron, my hemoglobin was steadily going up and we were pleased. About 4 weeks after starting the iron, I woke up to get ready for work and urinated black. I notified my hematologist. He had a list of labs he wanted drawn immediately. I had my labs done that day, a Sunday or Monday.
That Thursday, May 22, 2014, I was working (my wife and I are nurses). It was towards the end of my shift and my wife happened to come and check on me. My doctor called while my wife and I were talking, he has an answer to all of this. It’s Paroxysmal Nocturnal Hemoglobinuria. Right away, I think, “awesome! An answer!” I was relieved. I then googled “Paroxysmal Nocturnal Hemoglobinuria Hemoglobinuria: (hee-muh-gloe-buh-NYOOR-ee-uh) The presence of hemoglobin in the urine. ” as he began explaining the disease.
My heart sank in disbelief. The only cure for PNH is a bone marrow transplant bone marrow transplant: A bone marrow transplant (BMT) is also called a stem cell transplant (SCT) or hematopoietic stem cell transplant (HSCT).The procedure replaces unhealthy blood-forming stem cells with healthy ones and offers some patients the possibility of a cure. But for many patients, a BMT is not an option due… (Johns Hopkins Medicine,n.d.). Immediately I came upon information regarding the lifespan of a PNH patient. This narrative has changed over the last 6 years as more treatments are tested and one more medication (Ultomiris) has been approved for treating PNH. At the time of my diagnosis, there was a lot of as my physician says, "inaccurate" information regarding life expectancy of PNH patients, since so much information online referenced patients living with PNH before treatment with Soliris existed.
I decided while writing this that I would Google “PNH Patient Lifespan” and see what I found. The information I found at Johns Hopkins Medicine(n.d.) stating “the median survival after diagnosis is 10 years" is similar to what I initially read the day I was diagnosed; however, Johns Hopkins Medicine (n.d.) continues the same sentence to say "however, now that effective therapy exists, most PNH patients should be able to live a normal life expectancy". According to the Aplastic Anemia Aplastic Anemia: (ay-PLASS-tik uh-NEE_mee-uh) A rare and serious condition in which the bone marrow fails to make enough blood cells - red blood cells, white blood cells, and platelets. The term aplastic is a Greek word meaning not to form. Anemia is a condition that happens when red blood cell count is low. Most… & MDS International Foundation [AAMDSIF] (n.d.a) PNH patients “will soon have a lifespan that is normal compared with people their own age”. Six years after my diagnosis, I am excited to post this information regarding current PNH life expectancy because the experience and fear of reading what I did that initial day defined my life and bred fear for a long time.
Remembering most of the initial conversation of my diagnosis is a blur. At the time it was all white noise and disbelief. Questions and connecting dots. My physician was patient and explained the PNH diagnosis inside and out. He answered every question my wife and I had. After a solid 25-minute phone call that night, he asked us to come to his office the next day. There, we sat for another hour and a half and reviewed the disease extensively. These were questions I had for my physician at the time of diagnosis and I have answered them below.
- "What test was done that showed that I had PNH?" PNH is diagnosed using a blood test called flow cytometry flow cytometry: (sy-TOM-uh-tree) A laboratory test that gives information about cells, such as size, shape, and percentage of live cells. Flow cytometry is the test doctors use to see if there are any proteins missing from the surface of blood cells. It is the standard test for confirming a diagnosis of paroxysmal… . AAMDSIF (n.d.b) explains that flow cytometry is the "gold standard" for diagnosis as it is able to identify the missing proteins on a patient’s blood cells. (I encourage everyone reading this to research flow cytometry and how it works, it is fascinating.)
- "Have all of my blood cells mutated into PNH cells?" My physician explained that the percentage of cells in my body which are missing proteins are referred to as my PNH Clone Clone: To make copies. Bone marrow stem cells clone themselves all the time. The cloned stem cells eventually become mature blood cells that leave the bone marrow and enter the bloodstream. Count. A PNH patient's clone count can vary from 0.01 %- 100% (PNH National Service, 2020a). My PNH clone count is in the high 80%. According to the PNH National Service (2020a) the PNH clone is accurately determined by using flow cytometry to measure the percentage of the patients PNH granulocytes as these cells are not affected by hemolysis hemolysis: (hi-MOL-uh-suss) The destruction of red blood cells. like the red blood cells are.
- "I read that PNH can cause blood clots?" Yes. Per the AAMDS (n.d.d) at a minimum one of three PNH patients will suffer from blood clots. The PNH National Service (2020b) states that half of all PNH patients will suffer blood clots and per Johns Hopkins Medicine(n.d.) blood clots are the leading cause of death in PNH patients. Patients with PNH form blood clots due to what researchers believe are abnormally sticky platelets (AAMDSIF, n.d.d). However, both Johns Hopkins Medicine (n.d.) and the PNH National Service (2020b) state that treatment with Eculizumab Eculizumab: Eculizumab (Soliris ®) is given as an IV into a vein at the doctor’s office or at a special center. The procedure usually takes about 35 minutes. You will probably get an IV once a week for the first 4 weeks. Starting in the 5th week, you will get a slightly higher dose of Soliris every 2 weeks. … (Soliris) reduces risk for blood clots in PNH patients as well as other complications caused by PNH! If you didn't know already, Soliris was the first drug approved to treat PNH in patients by the FDA and the EMEA until 2018 when the longer acting complement inhibitor Ultomiris was approved by the FDA for PNH treatment (AAMDSIF, n.d.e).
After explaining and answering our questions my physician set out a plan for what was to come before starting treatment for my PNH. First, I would need a bone marrow biopsy bone marrow biopsy: A medical procedure to remove a small piece of solid bone marrow using a needle that goes into the marrow of the hip bone. The solid bone marrow is examined for cell abnormalities, the number of different cells and checked for scarring of the bone marrow. to confirm that I did not have aplastic anemia along with my PNH. Both PNH and Aplastic Anemia are bone marrow failure bone marrow failure: A condition that occurs when the bone marrow stops making enough healthy blood cells. The most common of these rare diseases are aplastic anemia, myelodysplastic syndromes (MDS) and paroxysmal nocturnal hemoglobinuria (PNH). Bone marrow failure can be acquired (begin any time in life) or can be… diseases, and per the AAMDSIF (n.d.c) 10 of every 100 aplastic anemia patients will develop PNH, as well some with PNH will develop Aplastic Anemia. According to Johns Hopkins Medicine (n.d.) "up to 30% of newly diagnosed cases of PNH evolve from aplastic anemia". The bone marrow biopsy showed I do not have aplastic anemia.
After completing my bone marrow biopsy, my physician recommended that my wife and I travel to Duke University to consult with a PNH specialist. During this consultation, the specialist reviewed my lab work, answered any questions and gave his recommendations for beginning treatment. His recommendation, Eculizumab (Soliris) was at the time the only approved treatment for PNH. Soliris reduces the breakdown of a PNH patient's blood cells by blocking the
complement system
complement system:
A group of proteins that move freely in the bloodstream. These proteins support (complement) the work of white blood cells by fighting infections.
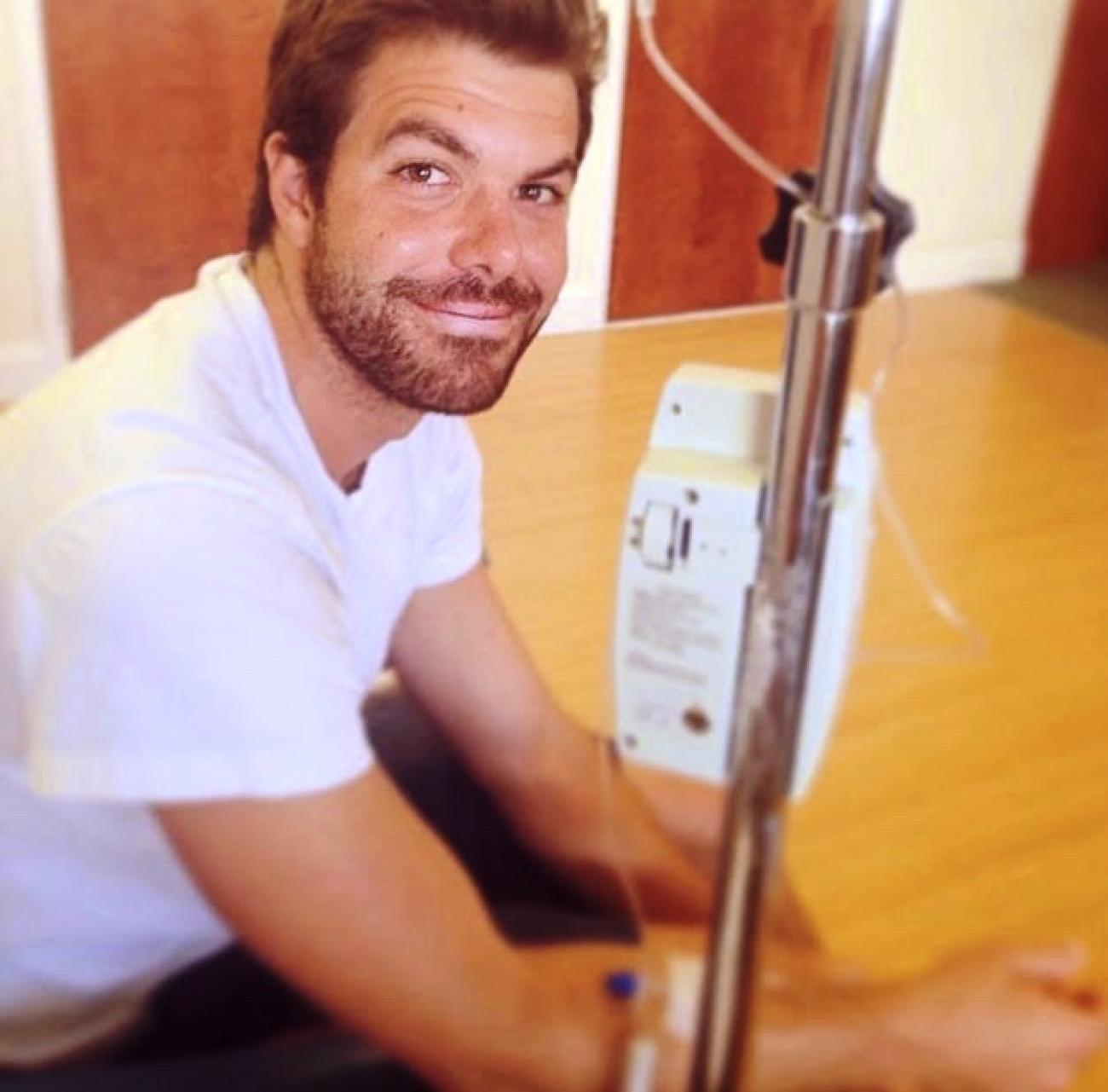
, which is responsible for the hemolysis in PNH patients (AAMDSIF, n.d.d) After completing a loading dose schedule, Soliris maintenance dose is administered every fourteen days intravenously (PNH National Service, 2020). We would return home from Duke with the plan to begin treatment with Soliris.
Before beginning Soliris—
- Vaccinate with Meningococcal Vaccine— Per the Centers for Disease Control and Prevention[CDC](2019) complement inhibitors including Soliris increase a patient's risk for meningococcal infections 1000 to 2000 times, so patients must be vaccinated two weeks prior to starting treatment to protect against meningococcal disease. If you are curious about the CDC recommendations of meningococcal vaccine for patients taking complement inhibitor therapy visit here.
- Get Approval from insurance for Soliris— the drug is EXPENSIVE, very very EXPENSIVE— a bill I found while researching price showed the cost of a Soliris infusion was charged to my insurance at $40,770.00 (and let’s not forget, this is every two weeks). In my experience, prior authorization from insurance is a must. My wife and I had to work very closely with my physician's office to be sure we had everything approved by insurance before I could start my Soliris.
In early July 2014, I started treatment with Soliris for Paroxysmal Nocturnal Hemoglobinuria.
I’ll continue my story in a future update.
-----
This story was taken from Josh and his wife's blog about living with PNH. You can follow their story here at www.dayfifteen.com.
Works Cited
Aplastic Anemia & MDS International Foundation. (n.d.a) How long do I have to live?
https://www.aamds.org/questions/how-long-do-i-have-live
Aplastic Anemia & MDS International Foundation. (n.d.b) Diagnosis.
https://www.aamds.org/diseases/pnh/diagnosis
Aplastic Anemia & MDS International Foundation. (n.d.c) Paroxysmal Nocturnal Hemoglobinuria(PNH).
https://www.aamds.org/diseases/pnh
Aplastic Anemia & MDS International Foundation. (n.d.d) Treatments.
https://www.aamds.org/diseases/pnh/treatments
Centers for Disease Control and Prevention. (2019, May 31). Managing the Risk of Meningococcal
Disease among Patients who receive Complement Inhibitor Therapy.
https://www.cdc.gov/meningococcal/clinical/eculizumab.html
Cleveland Clinic. (02/02/2018). Low Hemoglobin.
https://my.clevelandclinic.org/health/symptoms/17705-low-
hemoglobin
Johns Hopkins Medicine. (n.d.) Paroxysmal Nocturnal Hemoglobinuria(PNH).
https://www.hopkinsmedicine.org/kimmel_cancer_center/cancers_we_treat/bone_marrow_failure_dis
orders/paroxysmal_nocturnal_hemoglobinuria.html
PNH National Service, Leeds & London. (2020a). Frequently Asked Questions.
https://www.pnhleeds.co.uk/patients/what-is-pnh/frequently-asked-questions/
PNH National Service, Leeds & London. (2020b). Overview of PNH.
https://www.pnhleeds.co.uk/professionals/overview-of-pnh/
PNH National Service, Leeds & London. (2020c). Eculizumab Treatment.
https://www.pnhleeds.co.uk/patients/treatments/eculizumab-treatment/

